HOLEP
HoLEP is an advanced, minimally invasive, surgical laser treatment for patients with urinary symptoms due to a benign enlarged prostate.
Holmium Laser Enucleation of Prostate (HoLEP)
The Specialist Surgeons at The Reading Urology Partnership are pleased to offer Holmium Laser Enucleation of Prostate (HoLEP) as an alternative to Transurethral Resection of the Prostate (TURP).
It is used to treat patients with urinary symptoms due to benign prostate enlargement (Benign Prostatic Hypertrophy, BPH).
Instead of using electrical energy, it uses a high-energy laser to remove the core of the prostate from inside the gland to create an open channel, whilst avoiding the muscles and nerves that are important to maintain urinary continence and erectile function. The surgical procedure is performed with a special endoscope passed through the urethra.
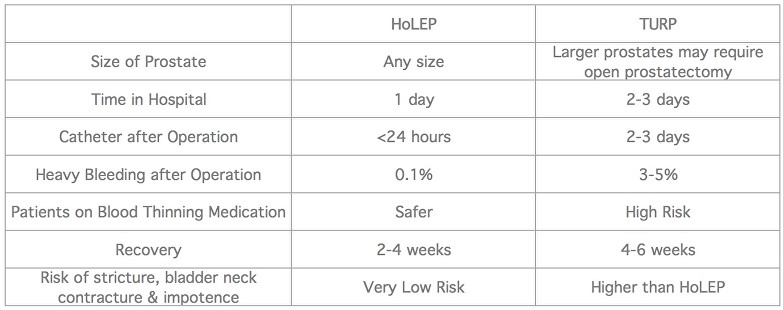
Holmium laser enucleation of the prostate (HoLEP) is particularly useful for larger prostates. It does remove more prostate tissue than a TURP would but with less chance of bleeding and a shorter recovery time. There is an added advantage of also doing vapourisation, resection or a combination of vapo-resection with the Holmium Laser.
HoLEP (Holmium laser enucleation of Prostate is the most advanced laser technique currently available and has been recommended by the National Institute of Clinical Excellence, NICE in its guidelines.
In contrast to Green Light laser Vapourisation of the prostate it has been rigorously evaluated in randomised trials. It is a size independent procedure suitable for any prostate in experienced hands, and highly effective at treating urinary retention.
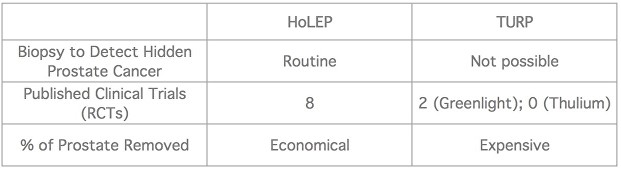
The High Power Holmium Laser separates the central part of prostate from the surrounding fibrous covering (capsule) and this procedure is nearly bloodless as the laser beam when cuts the gland also seals the blood vessels. The separated part of the prostate is then pushed into urinary bladder and is cut into small pieces and sucked out by a special machine (Morcellator). The smaller pieces of the prostate are sent for biopsy to detect prostate cancer.
HOLEP Procedure
This operation involves the removal of obstructing prostate tissue using a laser, followed by temporary insertion of a catheter to help the bladder drain normally. The procedure is usually carried out under a general anaesthetic (you are asleep). On average, the procedure takes 60-180 minutes, depending on the size of your prostate, and necessitates an over-night stay with a catheter in place.
HoLEP is suitable for any man with a blockage of his urinary system.
There are fixed priced quotes available on request. Please contact us on 0118 920 7040.
You have been diagnosed with urinary outflow obstruction (trouble passing urine) caused by an enlarged prostate or in urinary retention. HoLEP is a treatment recommended for men with large prostates and is probably safer for men on medications to thin the blood such as warfarin, aspirin or clopidogrel.
Alternative treatment options include: medication; use of a catheter to bypass the obstruction; observation; conventional transurethral resection (TURP) surgery, or an open operation. There are some newer alternatives such as Rezum, Urolift and Prostate Artery Embolisation (PAE). You could discuss suitability of procedure options with the consultant during your appointment.
If you are taking the blood-thinning agent clopidogrel on a regular basis, you must stop 7 days before your admission for the procedure as this drug can cause increased bleeding after prostate surgery. You can resume taking clopidogrel safely about 10 days after you get home. If you are taking warfarin or aspirin to thin your blood, you should ensure that the Urology staff are aware of this well in advance of your admission.
You will normally be asked to attend a pre-operative appointment before to assess your general fitness, to screen for the carriage of MRSA and to perform some health checks.
Please be sure to inform your pre-op assessment nurse or surgeon/anaesthetist in advance of your surgery if you have any of the following:
- An artificial heart valve
- A coronary artery stent
- A heart pacemaker or defibrillator
- An artificial joint
- An artificial blood vessel graft
- A neurosurgical shunt
- Any other implanted foreign body
- A regular prescription for warfarin, aspirin or clopidogrel (Plavix®)
- A previous or current MRSA infection
- A high risk of variant – CJD (if you have received a corneal transplant, a neurosurgical dural transplant or previous injections of human derived growth hormone).
You will usually be admitted on the day of your surgery. You will be asked not to eat or drink for 6 hours before surgery. After admission, you will be seen by members of the medical team which may include the consultant, anaesthetist and nursing staff.
At some stage during the admission process, you will be asked to sign the consent form giving permission for your operation to take place. This shows that you understand what is to be done and confirms that you wish to proceed. Make sure that you are given the opportunity to discuss any concerns and to ask any questions you may still have before signing the form.
Immediately before the operation, you may be given a pre-medication by the anaesthetist, which may make your mouth dry and make you feel pleasantly sleepy.
A full general anaesthetic will be used. You can discuss any anaesthetic related concerns with the anaesthetist prior to the procedure. In addition, you will usually be given an injectable antibiotic before the procedure, after checking for any drug allergies.
Once you are asleep, a laser is used to separate the obstructing prostate tissue from its surrounding capsule and to push it in large chunks into the bladder. An instrument is then used through a telescope device to remove the prostate tissue from the bladder. A catheter is normally left to drain the bladder at the end of the procedure.
In general terms, you should expect to be told how the procedure went and you should:
- Ask if what was planned was done and achieved.
- Let the medical staff know if you are in any discomfort.
Ask what activities you can and cannot do. - Feel free to ask any questions or discuss any concerns with the ward staff and members of the surgical team.
- Ensure that you are clear about what has been done and what you should do next.
- There is always some bleeding from the prostate area after the operation. The urine is usually clear of blood within a few days, although some patients lose more blood for longer. It is very rare to require a blood transfusion after laser surgery.
- You should drink as much fluid as possible in the first 12 hours after the operation because this helps to clear the urine of any blood more quickly. Sometimes, fluid is flushed through the catheter to clear the urine of blood.
- You will be able to eat and drink on the same day as the operation when you feel able to.
- The catheter is generally removed on the morning after surgery. At first, it may be painful to pass your urine and it may come more frequently than normal. Any initial discomfort can be relieved by painkillers such as Paracetamol and the frequency usually improves within a few days.
- Some of your symptoms, especially frequency, urgency and getting up at night to pass urine, may not improve for several months because these are often due to bladder over-activity (which takes time to resolve after prostate surgery) rather than prostate blockage. Since a large portion of prostate tissue is removed with the laser technique, there may be some temporary loss of urinary control until your pelvic floor muscles strengthen and recover. You will be taught pelvic floor exercises following surgery to help achieve this.
- It is not unusual for your urine to turn bloody again for the first 24-48 hours after catheter removal. Some blood may be visible in the urine even several weeks after surgery but this is not usually a problem.
- Let your nurse know if you are unable to pass urine and feel as if your bladder is full after the catheter is removed. Some patients, particularly those with small prostate glands, are unable to pass urine at all after the operation, due to temporary swelling of the prostate area. If this should happen, we normally insert a catheter again to allow the swelling to resolve and the bladder to regain its function.
- Usually, patients who require re-catheterisation go home with a catheter in place and then return within a couple of weeks for a second catheter removal, which is successful in almost all cases.
As with any other medical procedure there is a potential for side effects. You should be reassured that, although all these complications are well recognised, the majority of patients do not suffer any problems after a urological procedure. The side effects you might experience include:
Common (greater than 1 in 10)
- Temporary mild burning, bleeding and increased frequency of urination after the procedure.
- No semen is produced during an orgasm in approximately 95% of men if the prostate is fully enucleated.
Treatment may not relieve all the urinary symptoms. - Poor erections (impotence in approximately 5%).
Infection of the bladder, testes or kidney requiring antibiotics. - Possible need to repeat treatment later due to re-obstruction (approx. 1-2%).
Injury to the urethra causing delayed scar formation. - Loss of urinary control (incontinence) which reduces within 6 weeks (5%). This can usually be improved with pelvic floor exercises.
Occasional (between 1 in 10 and 1 in 50)
- May need self catheterisation to empty bladder fully if bladder weak.
- Failure to pass urine after surgery, requiring a new catheter.
- Bleeding, requiring a return to theatre and/or blood transfusion (less than 1%).
Rare (less than 1 in 50)
- Finding unsuspected cancer in the removed tissue which may need further treatment.
- Retained tissue fragments floating in the bladder which may require a second telescopic procedure for their removal.
- Very rarely, perforation of the bladder requiring a temporary urinary catheter or open surgical repair.
- Persistent loss of urinary control which may require a further operation (1%).
When you leave hospital, you will be given a discharge summary of your admission. This holds important information about your inpatient stay and your operation. If you need to call your GP for any reason, or to attend another hospital, please take this summary with you to allow the doctors to see details of your treatment. This is particularly important if you need to consult another doctor within a few days of your discharge.
Most patients feel tired and below par for a week or two because this is major surgery.
You may notice that you pass very small flecks of tissue in the urine at times within the first month as the prostate area heals. This does not usually interfere with the urinary stream or cause discomfort.
About 1 man in 5 experiences bleeding some 10-14 days after getting home. This is due to scabs separating from the cavity of the prostate. Increasing your fluid intake should stop this bleeding quickly but, if it does not, you should contact your GP or call 11 Kendrick Road during working hours or the Berkshire Independent Hospital out of hours. In the event of severe bleeding, passage of clots or sudden difficulty in passing urine, you should contact your GP immediately please follow the same advice as above and you may need to be readmitted into hospital.
Removal of your prostate should not adversely affect your sex life provided you are getting normal erections before the surgery. Sexual activity can be resumed as soon as you are comfortable; usually after 3-4 weeks.
It is often helpful to start pelvic floor exercises as soon as possible after the operation since this can improve your control when you get home.
The symptoms of an overactive bladder may take three months to resolve, whereas the flow is improved immediately.
The results of analysis on any tissue removed will be available after 7-10 days and you and your GP will be informed of the results by letter. You will be reviewed in the Outpatient Clinic 2-3 months after your surgery which may include a flow rate and bladder scan to help assess the effects of the surgery.
Most patients require a recovery period of 3-4 weeks at home before they feel ready for work. We recommend 3-4 weeks rest before resuming any job, especially if it is physically strenuous and you should avoid any heavy lifting during this time.
It is your responsibility to ensure that you are fit to drive following your surgery. You do not normally need to notify the DVLA unless you have a medical condition that will last for longer than three months after your surgery and may affect your ability to drive. You should, however, check with your insurance company before returning to driving. Your doctors will be happy to provide you with advice on request.
Please look at these external links for further information on HoLEP and additional support:
National Institute of Clinical Excellence, NICE
BAUS (British Association of Urological Surgeons) Patient Information Sheet
Laser Prostatectomy, Wikipedia
Prostate Laser Surgery, The Mayo Clinic, USA
Royal Berkshire Hospital HoLEP. Patient Information Sheet
Next Steps
Get fast access to leading specialists for the swift diagnosis and treatment of urological conditions in a private clinic environment.
If you would like more information or wish to arrange a consultation with one of our specialist consultant urological surgeons then please either Call 0118 920 7040 or complete the form below.
Insured patients
Contact your GP and ask for a referral to the Urology Partnership.
All consultations, investigations and treatments are covered by major insurance companies (depending on policy).
Funding your own treatment
Self-funding initial consultation fee is £205. Follow up fees are £165.
Consultation charges are exclusive of any tests and other investigations that the consultant may wish to carry out.


